Chemotherapy rewires gut bacteria to curb metastasis
22 January 2026
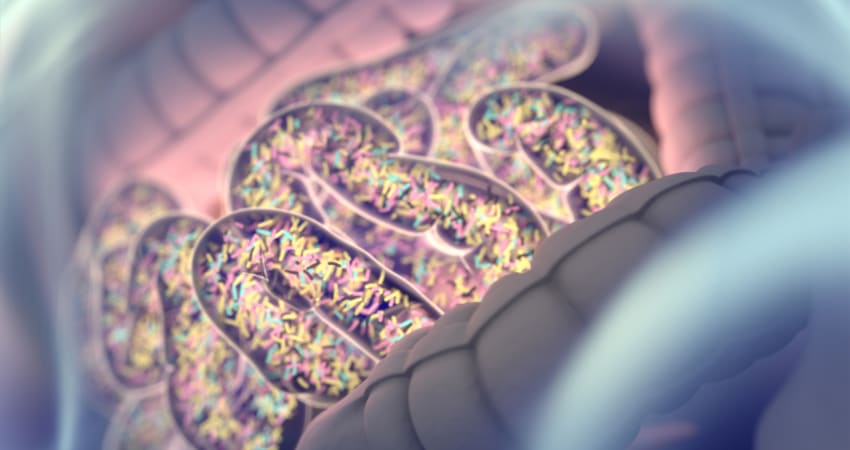 Credit: Getty Images/ChrisChrisW
Credit: Getty Images/ChrisChrisWBy Olivia Bowthorpe
Chemotherapy does more than kill cancer cells – it may also rewire the body's defences to stop cancer spreading in the first place.
A new study has uncovered an unexpected chain reaction: chemotherapy damages the gut lining, altering the microbiota, a well-known side-effect. This triggers bacteria to then produce a compound that travels through the bloodstream to the bone marrow, priming the immune system to attack metastases more effectively, say researchers.
The research looked at high-risk stage II and stage III colorectal cancer patients receiving standard chemotherapy after surgery. Whilst the treatment reduces recurrence risk, many patients still develop liver metastases – a pattern that prompted researchers at the University of Lausanne, Switzerland, to investigate what else might be happening beyond tumour cell death.
Bacteria that process the amino acid tryptophan become more common and produce higher levels of a compound called indole-3-propionic acid (IPA), they discovered.
IPA moves from the gut into the bloodstream and reaches the bone marrow where it changes how some immune cells develop, the team report in Nature Communications.
This reduces the number of immunosuppressive monocytes, which normally help cancer cells evade destruction by the immune system. With fewer of these cells, T cells become more active and better able to attack cancer.
“We were surprised by how a side effect often seen as collateral damage of chemotherapy can trigger such a structured systemic response," said Ludivine Bersier, first author and researcher at the University of Lausanne.
"By reshaping the gut microbiota, chemotherapy sets off a cascade of events that rewires immunity and makes the body less permissive to metastasis.”
In tests on mice, this immune shift was seen to create a state that resisted liver metastases for weeks after a single chemotherapy cycle. Giving IPA directly to mice had a similar protective effect.
Patient samples also suggested that IPA levels increased after chemotherapy and were linked with lower monocyte counts, which is linked to better outcomes. This effect varied between patients, perhaps due to differences in gut bacteria, diet, or other medications.
"Up to 50% of colorectal cancer patients develop intestinal mucositis after the first round of chemotherapy, which may trigger the local and systemic release of cytokines, growth factors, and bacterial-derived products influencing subsequent metastatic relapse," the authors write.
Co-author, Professor Tatiana Petrova, commented: “This work shows that the effects of chemotherapy extend far beyond the tumour itself. By uncovering a functional axis linking the gut, the bone marrow and metastatic sites, we highlight systemic mechanisms that could be harnessed to durably limit metastatic progression.”
The team believe that maintaining healthy gut bacteria may help maximise treatment benefits, and raise concern over the use of broad-spectrum antibiotics around the time of surgery, as these could reduce IPA production and weaken this beneficial immune response.
Reference: Nat Commun DOI: 10.1038/s41467-025-67169-7
You might also like
